Close Coverage Gaps. Reduce Churn. Protect Revenue.
Having facilitated over 5 million interactions, Advocatia’s all-in-one platform simplifies eligibility and enrollment at scale, giving healthcare organizations the tools they need to increase coverage, strengthen compliance, and improve outcomes for your patients, members, and bottom line.
Every Step Covered on One Unified Platform
Advocatia brings together Medicaid navigation, eligibility screening, intake, follow-up, and reporting into one seamless experience. Built for patients, members and staff, it helps healthcare teams work more efficiently, connect more people to the support they qualify for, and track results every step of the way.
Automated Screening
Identifies 1,000+ benefit options (Medicaid, SNAP, WIC, etc.) in seconds to ensure maximum coverage.
Self-Service Intake
Individuals can upload documents and e-sign forms anytime, making it easier to get the information your staff needs, faster.
Automated Follow-Up
Whether it's your team reaching out or ours, text, email, and self-service follow-ups are automated to boost completion rates.
Staff-Assisted Workflows
Seamless workflows and interface for financial counselors to complete and submit applications efficiently.
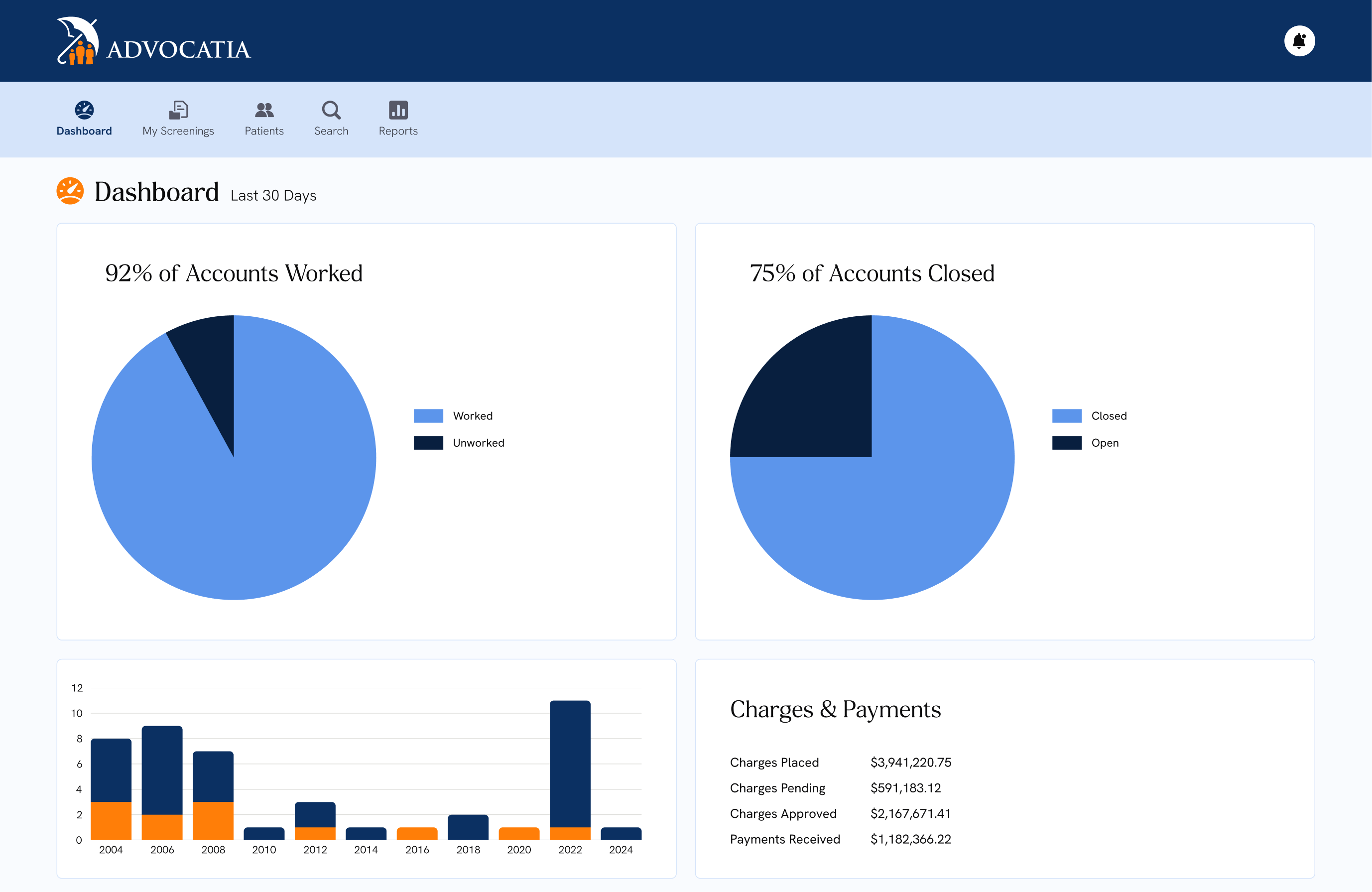
Data & Reporting
Integrates with your existing systems to track outcomes, ensure compliance, and build trust with your teams.
Results You Can Trust
5.5 million+ engaged individuals

Helps teams manage 30% more patients
33% reduction in processing time

4.9/5 star user rating
Recognized by Winner’s Circle, Best Patient Cost Savings, and SOC 2 Type 2



Designed for Coverage, Compliance, and Growth
Maximize reimbursement, minimize leakage
From Medicaid to charity care, we help you capture every dollar tied to eligible patients and members, boosting ROI without adding headcount.
Streamline complex, manual workflows
Public program enrollment is notoriously fragmented. We automate outreach, eligibility, and document collection so your teams can focus on care.
Reduce uncompensated care and churn
By proactively connecting more individuals to the coverage they qualify for, you can improve retention, protect your revenue and ultimately support healthier populations.
Deliver a seamless, human-centered experience
Whether it’s bedside, post-discharge, or fully self-service, our tools meet people where they are, turning a high-friction process into a supportive one.

Ready to experience the difference?
Let’s work together to simplify benefits enrollment and achieve measurable impact.

